Dementia treatment is changing faster than most people realize. A new study points to two familiar cancer drugs with a surprising side job. They seem to quiet the brain storms that steal memory in mice. If this holds in people, dementia treatment could get a fresh jolt of hope.
Old Drugs, New Clues
Scientists at UCSF and Gladstone sifted through how Alzheimer’s rewrites genes in the brain. They mapped those changes like a fingerprint, then searched for drugs that flipped the pattern. Their compass was the Connectivity Map, a vast index of drug signatures and cellular responses. The search kept circling two names already familiar to oncologists: letrozole and irinotecan. Both are FDA approved, which shortens the runway for studies outside cancer. The team also combed medical records from treated patients and tracked later Alzheimer’s diagnoses.
People exposed to these drugs showed a lower chance of developing the disease. That kind of real-world hint doesn’t prove cause, yet it nudges the question forward. Together, these clues suggest a fresh angle for dementia treatment that starts with data. Not a single lab bench, at least not at first. Then the team checked the hunch the hard way, with animals and timed tasks. You want moves on a maze, not just a heat map on a screen. Numbers on paper matter, yet behavior tells you if the brain can rally.
Dementia treatment
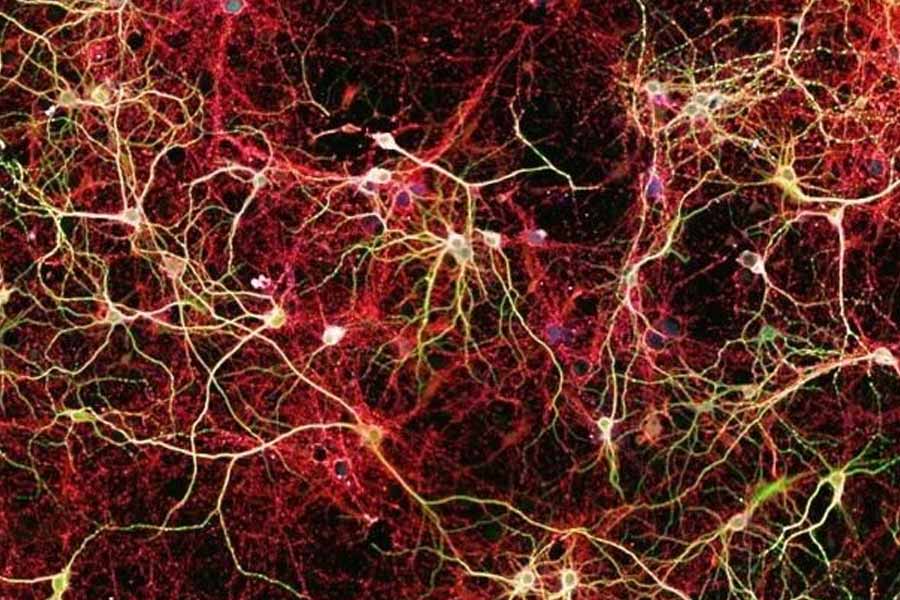
After the database hunt came the hard test: living brains. In mouse models of Alzheimer’s, the drug pair reversed several hallmarks of the disease. Clumps of tau protein shrank, easing the burden that chokes nerve cells. The mice also performed better on tasks that probe learning and memory. Letrozole seemed to steady neurons, while irinotecan leaned into the support crew, the glia. Two drugs, two targets, one coordinated push. It’s a simple idea with a lot of practical weight behind it.
Both drugs already have dosing playbooks, safety notes, and a supply chain. That makes real trial design faster, though still careful by necessity. If verified in people, this could broaden dementia treatment from single targets to tuned combinations. The effect wasn’t a cure, more like easing a heavy backpack. That lighter load let circuits talk a bit clearer, at least in tests. The images from the study showed fewer tau tangles crowding the tissue. You could almost sense the relief in those slices under the scope.
Two Paths, One Brain
Why might this pairing help at all? Alzheimer’s doesn’t move through one pathway or one misbehaving molecule. It scatters trouble across networks, bending many switches at once. Single drugs often fight on narrow ground and lose momentum. A combination can press on different levers without overdosing either one. Here, neurons get extra stability, while glia get a nudge to restore balance. That two-front strategy matches what biologists see in diverse brain cell types. The study’s computational lead described the analysis as finally meeting the puzzle head-on.
Patterns across genes guided the shortlist, then biology had the last word. It’s early, still, yet the logic feels grounded and testable for dementia treatment. Not a silver bullet, more a well aimed toolkit. Drug development often chases a single villain because trials are cleaner that way. Brains rarely play along, which is why fresh angles matter. Repurposing also trims years off logistics and manufacturing headaches. Labs can focus on dosing ranges and timing instead of reinventing chemistry.
From Mice to Us
Mice are a starting line, not the finish. These medications carry side effects that cancer teams already know well. Any repurposing will need fresh safety work, and probably new dosing playbooks. Human trials come next, with smart guardrails and tight monitoring. There’s also the question of who benefits most, and who does not. The researchers think gene expression profiles can guide choices patient by patient. Imagine a clinic matching brain signatures to the best tested mix. That’s the promise: more precision, less guesswork, and safer care. The need is massive, with more than 55 million people living with Alzheimer’s today.
Without better answers, that number may more than double within 25 years. Every delay carries real human costs for families, caregivers, and patients. This work appears in Cell, a journal that spends real effort vetting data. Publication isn’t a victory lap, only a public ledger of methods and results. Even so, the idea that an existing pair might reshape dementia treatment is hard to ignore.
Hope is not a plan, yet it drives people to show up for trials. If the benefits hold, clinics could pivot faster than with a brand-new molecule. Insurance frameworks would still need updates before any off-label wave begins. Regulators will want careful endpoints, not only memory tests but daily function. Caregivers need treatments that ease nights, reduce wandering, and buy calm. Small wins add up when a household is stretched thin. That’s where this line of work could quietly change lives.